Irritable Bowel Syndrome and Interstitial Cystitis
 Interstitial cystitis and irritable bowel syndrome (IBS) are chronic pelvic pain disorders and, not surprisingly, often coexist. Research studies have demonstrated that 40 to 60% of IBS patients exhibit symptoms of IC while up to 52% of IC patients also have symptoms consistent with IBS.1 For patients who struggle with both conditions, the connection is often baffling until you consider the role of the nerves.
Interstitial cystitis and irritable bowel syndrome (IBS) are chronic pelvic pain disorders and, not surprisingly, often coexist. Research studies have demonstrated that 40 to 60% of IBS patients exhibit symptoms of IC while up to 52% of IC patients also have symptoms consistent with IBS.1 For patients who struggle with both conditions, the connection is often baffling until you consider the role of the nerves.
The organs of the pelvis communicate in a process known as “neural cross-talk” to maintain normal bladder, bowel and reproduction function. Yet, in a surprising twist, these normal communication pathways can also convey irritation. Researcher Michael Pezzone MD was one of the first to demonstrate bowel-bladder cross-sensitization. In animal studies, he showed that when the bowel was acutely irritated in a single event, the bladder showed signs of irritation and when the bladder was irritated, the bowel shows signs of irritation.
Yet, it was his research into longterm, chronic irritation that offered more revealing information. Long-term irritation of the bowel triggered some of the familiar symptoms of IC including increased frequency and decreased urinary volume, as well as evidence of inflammation and increased numbers and activation of mast cells in the bladder wall. Dr. Pezzone wrote “In other words, after colonic (bowel) irritation, the very nerves that carry signals for uncomfortable bladder sensation had become hypersensitive…” 1
How does this happen? It turns out that the bladder and bowels outgoing, afferent nerves meet and combine near the spine thus providing both access and opportunity for “cross-talk.” This was proven when Dr. Pezzone injected tracers into the bowel and bladder. He found BOTH sets of tracers in the same nerve cells in the dorsal root ganglia. Dr. Pezzone and his peers now suggest that chronic pelvic pain develops after an acute injury or chronic irritation to perhaps just one of the pelvic organs (i.e the bladder, the bowel or the reproductive tract), pelvic floor muscles, nerves and/or perhaps even the skin of the perineum. Other proximal organs or muscles can then become involved through this “crosstalk” sensitization pathway if the irritation/ inflammation persists.
Pelvic pain specialists agree that treatment should be focused on calming and soothing every condition in the pelvis (IC, IBS, endometriosis, vulvodynia) that is producing pain and/or discomfort.
IBS is not a disease
Irritable bowel syndrome is estimated to affect 3 to 20 percent of the population, with most studies ranging from 10 to 15 percent.2 However, less than one-third of people with the condition see a health care provider for diagnosis. 3 IBS affects about twice as many women as men and is most often found in people younger than 45 years.
According to the National Institutes of Health, “Irritable bowel syndrome is a functional gastrointestinal (GI) disorder, meaning it is a problem caused by changes in how the GI tract works. People with a functional GI disorder have frequent symptoms, but the GI tract does not become damaged. IBS is not a disease; it is a group of symptoms that occur together.”4
Heather Van Vorous, author of First Year: IBS, offered “IBS is considered a brain gut disorder and there are two aspects of that. The enteric nervous system is dysfunctional in people who have IBS. But, so is the way that the brain interprets messages from the enteric nervous system…We call it a hypersensitivity of the gut. That’s why stress and food are the two greatest triggers. They both affect the gut and the gut overacts to both of those things, creating the symptoms of IBS. It’s important that you realize that stress and diet doesn’t cause IBS but theydefinitely trigger the symptoms just like IC.”5
Some patients with irritable bowel syndrome struggle with painful cramping and diarrhea after eating certain foods or heavy meals while others struggle with chronic constipation and hard, lumpy stools. Patients may feel urgency to have a bowel movement or feel that their bowel movement is incomplete. Small, hard stools and/or straining to have a bowel movement can occur. Discomfort usually improves after having a bowel movement.
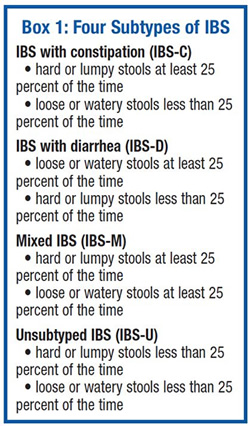
For IBS to be diagnosed, the symptoms must have started at least six months prior and must have occurred at least three days per month for the previous three months. Further testing is not usually needed though the health care provider may do a blood test to screen for other problems. Additional diagnostic tests may be needed based on the results of the screening blood test and for people who also have signs such as fever, rectal bleeding, weight loss, anemia or a family history of colon cancer, IBS or celiac disease. Based upon those findings, patients will be given a classification (see box 1).
What causes IBS?
The causes of IBS are still unclear though Dr. Pezzone has made a good case for pelvic organ cross-talk and neurosensitization. Some IBS patients can point to an initial bowel trauma, such as a severe case food poisoning, bacterial gastroenteritis, surgery or perhaps even childbirth. A brain-gut signaling problem or perhaps some GI motility issues may contribute in some cases. Slow motility can lead to constipation and fast motility can lead to diarrhea. Genetics could also play a role. Quite a few patients report food sensitivity issues, such as with foods high in caffeine, MSG, coffees, fats, etc.
Heather believes that the gastrocolic reflex, the normal message that the stomach sends to the colon after you’ve eaten that triggers a bowel movement, has become hypersensitive. She said “In people with IBS this reflex goes haywire. Their colon is contracting too much, too hard, too fast, or it’s in spasms or not contracting enough. They may have too few contractions, not strong enough, or be irregularly timed. This can then cause abdominal pain, diarrhea, constipation, bloating, and trapped gas. And that’s all stemming from the hypersensitive gastrocolic reflex.”
IBS Diet Modification Tips
IBS patients learn, fairly quickly that certain foods can trigger symptoms. Heather offered “There are two categories of foods that stimulate the gastrocolic reflex more than anything else. (1) Fats and (2) Insoluble fibers… It’s actually very easy to work around this.” Alcohol, caffeine, chocolate, artificial sweeteners, foods which produce gas and/or high acid foods can also be troublesome. Sounds a lot like the IC diet, doesn’t it?
But when you’re struggling with constipation, well meaning family members and physicians suggest loading up on high, insoluble fiber foods (i.e. bran, granola, greens, roughage, psyllium products etc.). The challenge, of course, is that these “insoluble fibers” are notoriously challenging to the more tender IBS gut. Heather said “Insoluble fiber is a huge GI stimulant. It sends the gastrocolic reflex out of control and can trigger spasms, cramps, and diarrhea.. and can also exacerbate constipation. If you don’t have IBS, insoluble fiber is great for constipation. If you do have IBS, it can make your gut spasm and make those contractions so irregular that it interferes with motility and worsens constipation.”
It’s the starchy, soluble fiber found oatmeal, pasta, rice, potatoes, tapioca, bananas that is more soothing for the bowel and gut of a typical IBS patient. According to Heather, soluble fiber regulates the gastrocolic reflex, thus calming painful muscle contractions of the gut. Soluble fiber also regulates water content in the bowel and can help with both diarrhea and constipation. She said “People get so confused. I spend my life telling people with constipation that soluble fibers won’t make them worse and that they aren’t “binding.”’ She cautioned “Never have insoluble fiber alone, on an empty stomach, or in large quantities all at once. Always have insoluble fibers with soluble fibers. Make yourself fried rice and add some veggies to that or a put vegetable sauce on pasta. Try cooking some fresh fruit in your oatmeal. Cooking breaks down insoluble fiber and so does cutting it up and pureeing it in the blender, which makes it a lot more tolerable. Cooked veggies are safer than raw. A fresh fruit smoothie is safer than a big, raw fruit salad.”
Many patients have also experienced IBS attacks after eating salad greens. Greens (i.e. lettuce, spinach, kale, chard) also contain insoluble fibers which can stimulate the gut. Heather advises patients to make soluble fiber the foundation of their meals and/or the first thing that they eat in a given meal, saving the insoluble fiber for the end of the meal. Want a salad? Eat it after you eat the bread!
For protein, focus on lean meats such as skinless chicken, turkey breasts, seafood or egg whites. Fatty red meats are a well known IBS trigger because they are high in fat and the proteins are hard to digest. Dairy products high in fat and protein can also be a trigger.
High acid fruits and veggies can trigger discomfort for both IC and IBS. It can help to remove the skins because that contains most of the insoluble fiber. Bananas, pears, mild sweet apples, some melon are reasonable to try. Water intake is also important. Soluble fiber needs water in the gut to work, especially for patients who struggle with constipation. You can find many more diet ideas and strategies on Heather’s website: www.helpforibs.com
Treatments
The treatments for IBS are quite similar to the treatments for IC in that they are designed to calm and soothe nerves though, in this case, the nerves of the gut rather than the nerves in the bladder.
• Fiber Supplements
Many physicians recommend using a fiber supplement to ease constipation. Surprisingly, psyllium products are not the first choice for IBS because they contain some insoluble fiber. Soluble fiber products, such as Acacia Fiber, seem to be better tolerated.
• Laxatives
Several types of laxatives are available to ease constipation, including bulk-forming laxatives, stimulants, osmotics, stool softeners, lubricants, calcium channel acitvators and saline laxatives. Please talk with your doctor about which form of laxative would be best for you depending upon your specific condition.
• Antidiarrheals
Antidiarrheals (i.e. Loperamide) can help reduce diarrhea by slowing the movement of stool through the colon.
• Antispasmodics
Antispasmodics (i.e. hyoscine, cimetropium, pinaverium) can help control colon spasms.
• Antidepressants
Both tricyclic antidepressants (TCA’s) and selective serotonin reuptake inhibitors (SSRIs) in low doses can help relieve IBS symptoms including abdominal pain. In theory, TCAs should be better for people with IBS-D and SSRIs should be better for people with IBS-C due to the effect on colon transit, but this has not been confirmed in clinical studies. TCAs work in people with IBS by reducing sensitivity to pain in the GI tract as well as normalizing GI motility and secretion.
• Lubiprostone (Amitiza).
Lubiprostone is prescribed for people who have IBS-C. The medication has been found to improve symptoms of abdominal pain or discomfort, stool consistency, straining, and constipation severity.
• Probiotics
Probiotics are live microorganisms, usually bacteria, that are similar to microorganisms normally found in the GI tract. Studies have found that probiotics, specifically Bifidobacteria and certain probiotic combinations, improve symptoms of IBS when taken in large enough amounts. But more research is needed. Probiotics can be found in dietary supplements, such as capsules, tablets, and powders, and in some foods, such as yogurt. A health care provider can give information about the right kind and right amount of probiotics to take to improve IBS symptoms.
• Managing Stress & Talk Therapy
Talking with a therapist may reduce stress and improve IBS symptoms. Two types of talk therapy used to treat IBS are cognitive behavioral therapy and psychodynamic, or interpersonal, therapy. Cognitive behavioral therapy focuses on the person’s thoughts and actions. Psychodynamic therapy focuses on how emotions affect IBS symptoms. This type of therapy often involves relaxation and stress management techniques.
• Hypnotherapy
In hypnotherapy, the therapist uses hypnosis to help the person relax into a trancelike state. This type of therapy may help the person relax the muscles in the colon.
• Mindfulness training
People practicing this type of meditation are taught to focus their attention on sensations occurring at the moment and to avoid worrying about the meaning of those sensations, also called catastrophizing. It’s important to remember that IBS isn’t considered a disease. It is a functional disorder and your job is to learn what works best in your gut. If stress is an issue that provokes frequent IBS attacks, then you must work on and build your stress management skills. If your diet is out of control and you’re eating foods notorious for triggering diarrhea, then it’s worth trying some of the diet suggestions offered in The First Year: IBS – An Essential Guide for the Newly Diagnosed.
If your symptoms are not improving, look for a medical care provider, such as a gastroenterologist, that specializes in functional disorders. They may find that missing piece to your puzzle! It’s worth the effort.
References
- Pezzone M. Chronic Pelvic Pain and the Overlap of Chronic Pelvic Pain Disorders. International Foundation for Functional Gastrointestinal Disorders. 2007
- Grundmann O, Yoon SL. Irritable bowel syndrome: epidemiology, diagnosis, and treatment: an update for health-care practitioners. Journal of Gastroenterology and Hepatology. 2010;25:691–699.
- Owyang C. Irritable bowel syndrome. In: Yamada T, ed. Textbook of Gastroenterology. 5th ed. Vol. 1. West Sussex, UK: John Wiley & Sons Ltd.; 2009: 1536–1573.
- Irritable Bowel Syndrome. National Digestive Diseases Information Clearinghouse. NIH Publication No. 12-693. July 2, 2012
- Irritable Bowel Syndrome and IC: Practical Suggestions to Help IC/IBS Patients Manage Their Bowel Syndromes. 2006 IC & PBS On-Line Patient Conference – June 20, 2006
Resources
- Irritable Bowel Syndrome – National Digestive Diseases Information Clearinghouse. NIH Pub No 12-693, July 2012. digestive.niddk.nih.gov
- The First Year: IBS – An Essential Guide for the Newly Diagnosed – Heather Van Vorous and David Posner – 2001
- Heather’s Tummy Fiber – Organic Acacia Fiber
- Helpforibs.com – Heather Van Vorous’s IBS support website.
- American Neurogastroenterology and Motility Society
- International Foundation for Functional Gastrointestinal
- Rome Foundation
Author: Jill H. Osborne MA
Created: Feb. 2013
Updated: Jan 2017