Managing Interstitial Cystitis & Bladder Pain Flares
IC/BPS patients often struggle with “IC flares,” a sudden and dramatic worsening of their bladder symptoms. Lasting from hours to weeks, IC flares can be unpredictable, disruptive and difficult to manage for both newly diagnosed and veteran IC patients. Flares can be triggered in many different ways that irritate the bladder wall, tighten pelvic floor muscles and/or sensitize nerves. Food related flares may be felt within minutes or hours of eating a risk food and may last a day or longer. A sex induced flare may occur 24-48 hours after intimacy and last for several days. Hormone induced flares, such as the flare which may occur during ovulation, may last just a few hours. The good news is that many IC flares are preventable and are often predictable.
Are you flaring right now?
Confused? Frustrated? Desperate for relief? Your first step is to try determine what kind of flare you are having. Did your flare after eating or drinking a food? Are you under intense stress?? Did you take a long car ride? Have sex?
When is your pain the worst?
- Pain BEFORE urination (that gets worse as you bladder FILLS with urine and feels better once you have emptied your bladder) points to your bladder wall.
- Pain AFTER urination points to your pelvic floor as the probable source of your flare.
- If pain is intense before and after urination, you may have a combination flare that is involving the bladder, muscles and nerves.
Bladder Wall Flares
Risk Factors
Patients with Hunner’s lesions and/or bladder wall subtypes are the most at risk for bladder wall flares. Long-term pelvic floor dysfunction can cause ischemia which damages the bladder and makes it more sensitive.
Triggers
- DIET – Foods and drinks high in acids, alcohol and/or caffeine can trigger bladder irritation. Patients who have just one coffee or soda a day often suffer the most because that daily acid wash is irritating the wounds on the bladder. Healing happens when you remove the irritant and protect the bladder. Learn more about the diet here!
- VITAMINS & SUPPLEMENTS – Multivitamins contain Vitamins C and B6, both infamous for irritating the bladder and creating discomfort. Patients do better when taking individual vitamins or a low acid multivitamin (Bladder Smart Low Acid Vitamins). Supplements containing cranberry and other forms of acid (i.e. apple cider vinegar) can also irritate even though it converts to alkaline after digestion.
- HORMONES – Drops in estrogen with birth control, Lupron use, perimenopause or menopause (Genitourinary Syndrome of Menopause) reduce the integrity of the bladder wall making it more vulnerable to irritation. Some women also struggle with an IC flare on the day that they ovulate and a few days before their period. These are usually predictable and short-term.
- CHEMICAL EXPOSURE – Some chemicals and/or medications can trigger an IC flare, especially cigarette smoke and vaping. Even second hand exposure increases the risk of irritation and bladder cancer.
- UTI – Infection is rare but possible, often in women struggling with recurring UTI after menopause. Start with a simple OTC UTI Test Kit to test your urine. If the test strips change color, then contact your physician so that you have your urine cultured and, if positive, receive antibiotics. If your home test kit is negative, a bladder wall flare is likely. If you EVER seen blood in your urine, experience fever, chills and/or low back pain, you should contact your physician immediately.
Rescue Plan
0-30 Minutes After The Flare Begins
- REST – If you’ve been in pain or discomfort for just thirty minutes, stop what you are doing, sit down, rest and use a heating pad for several minutes. Try to break the cycle of irritation and/or muscle tension before it worsens.
- HEAT – Heat can relax your muscles. The GingerBee Microwaveable Pad provides quick relief but will hold heat for about 20 minutes before you have to heat it up again. BodiHeat Heating Pads are one-time use pads ideal to use during work, traveling or driving. Consider soaking in a warm bathtub but do not use bubbles, fragrance or bath salts. Try putting a handful or two of baking soda in your bathwater instead.
At 30-60 Minutes: Focus on Your Urine
- DILUTE YOUR URINE – Water helps to flush toxins out of your body. Whenever a flare begins, take a look at your urine. It should be clear and pale yellow in color. If it’s dark or cloudy, you may be dehydrated. If so, try drinking a glass of water or, better yet, sip a glass of water over an hour. Look at the color again. If it’s still dark yellow, more water may be helpful.
- REDUCE URINE ACID LEVELS – If you’ve eaten an acidic food (i.e. coffees, green teas, sodas, citrus, tomato products), try using some Prelief, Tums or a 1/2 teaspoon of baking soda in a glass of water to alkalinize (aka reduce the acid levels) in your urine. If you’re on a salt limited diet, please talk with your doctor before using the baking soda method.
- HERBAL TEA – A cup of herbal chamomile or peppermint tea can be quite soothing to the bladder and bowel.
At 60 Minutes: Catching Pain Early
- BLADDER ANALGESICS – Over The Counter AZO Bladder Pain Relief Tablets, Pyridium and Prosed are urinary anesthetics that help to numb the bladder wall. These can be very effective in patients struggling with mild bladder symptoms. The latter two require prescriptions from your physician.
- OTC ANALGESICS – As an early intervention for MILD pain, ibuprofin (aka Advil, Motrin) or acetaminophen (Tylenol) might be worth trying though they shouldn’t be expected to control severe pain. Please note that Ibuprofin can cause stomach irritation and acetaminophen can irritate the liver if used in large amounts.
- BLADDER SPASMS – If you’re feeling bladder spasms (unusual flip floppy sensations or a strong spasm at the end of urination), a smooth muscle antispasmodic (i.e. Ditropan, Detrol) may be helpful. These are prescription medications that must be prescribed by your physician and may cause drowsiness. Again, a cup of peppermint or chamomile herbal tea may also lessen spasms.
- ALOE can have a soothing effect on the bladder wall, just as it can be soothing to a sunburn. There are several aloe products on the market. Looking for ones that are organic & anthraquinone free. We suggest AloePath® which combines aloe with Palmitoylethanolamide to calm nerves!
- CBD (Hemp or Medical Marijuana) may help reduce pain and relax muscles. Edibles or topical creams are preferred over inhalants.
At 2-4 Hours: Getting Serious About Symptoms
Pain is a message. Your bladder and/or pelvis are telling you that they are in distress. It’s important that you not push through the pain. This is the time to relax and focus on what will make you feel better.
- PAIN MEDICATION – If the pain or discomfort is getting worse, you may need to start using a pain medication that your doctor has prescribed. Using pain medication early, before the pain gets out of control, is ideal. Opioid medications are the mainstream of treatment for moderate to severe pain. They come in many varieties and strengths. Some are “short-acting” medications (i.e. Tylenol with codeine) that are effe tive for about four hours and can help manage short-term persistent pain. Other medications are “long- acting” time release formulas (i.e. Oxycontin) that are designed for use with chronic pain.
- SOOTHING FOODS – A glance at the latest IC diet research shows that there are some foods which seem to be particularly sooth-ing to the bladder. Focus on mild, comfort foods like chamomile tea, rice, potatoes, chicken, fresh breads, vanilla ice cream, vanilla milkshakes, pears, carrots, mushrooms, squashes, etc. Yes, this is a very mild diet because we don’t want to create more irritation.
At 24 Hours & Longer – As you continue the strategies used previously, the following medical interventions may be considered.
- RESCUE INSTILLATIONS – Rescie instillations (aka anesthetic cocktails) provide immediate and sustained pain relief for some patients. This simple instillation of medication into your bladder usually contains lidocaine or marcaine to numb the bladder wall, heparin as a bladder coating, a corticosteroid to help control inflammation and, perhaps, an antibiotic.
- HUNNER’S LESION TREATMENT – Severe, persistent bladder wall pain is often the result of untreated Hunner’s lesions. The good news is that when they are treated correctly with, pain and discomfort improves in the great majority of patients.
Pelvic Floor Muscle Flares
Risk Factors
Pelvic floor flares often occur in patients who struggle with previous injury, pelvic surgery, weakness or hypertonicity. Symptoms can include frequency, urgency, pressure and pain. Patients often report a pushing or pulling sensation in their pelvis. Muscles may become so tight that nerve pain occurs, such as sciatica, pins and needles, areas of numbness or persistent genital arousal disorder (a sudden painful arousal sensation). The classic sign of tight pelvic floor muscles is delay starting your urine stream, hesitating 5, 10, 15 seconds or longer before you can relax enough to release urine.
Triggers
- DRIVING/TRAVELING – The vibration of a car, bus or plane flight is notorious for triggering pelvic floor tension and/or spasms. IC patients frequently report that they cannot drive long distances without experiencing great discomfort. If you’re in an IC flare, it’s best to limit car travel to short distances.
- SEX – Sexual intercourse can trigger an IC flare. Men with IC may experience a searing pain at the moment of orgasm. Women with IC often feel their worst 24-48 hours after intercourse, with increased levels of frequency, urgency or pain. Men and women can also struggle with intense pelvic floor muscle spasms. Read more in the ICN Guide To Sex and Intimacy.
- EXERCISE – Exercise, particularly workouts that involve the pelvic area, can trigger yet more muscle tension. Bicycle seats put unusually high pressure on the pelvic floor muscles, thus exacerbating ICsymptoms. Other patients have reported that workouts that jar the pelvis, such as running or stair master, can provoke pain. Look for exercises that keep the hips level and are none jarring (i.e. swimming, walking, elliptical, rowing, yoga, pilates, etc.)
Rescue Plan
0-30 Minutes After the Flare Begins
- REST – If you’ve been in pain or discomfort for just thirty minutes, stop, rest and try to break the cycle of irritation and/or muscle tension before it worsens. Try using a heating pad on your lower belly to help relax your pelvic floor.
At 30-60 Minutes: Getting serious about your muscle tension
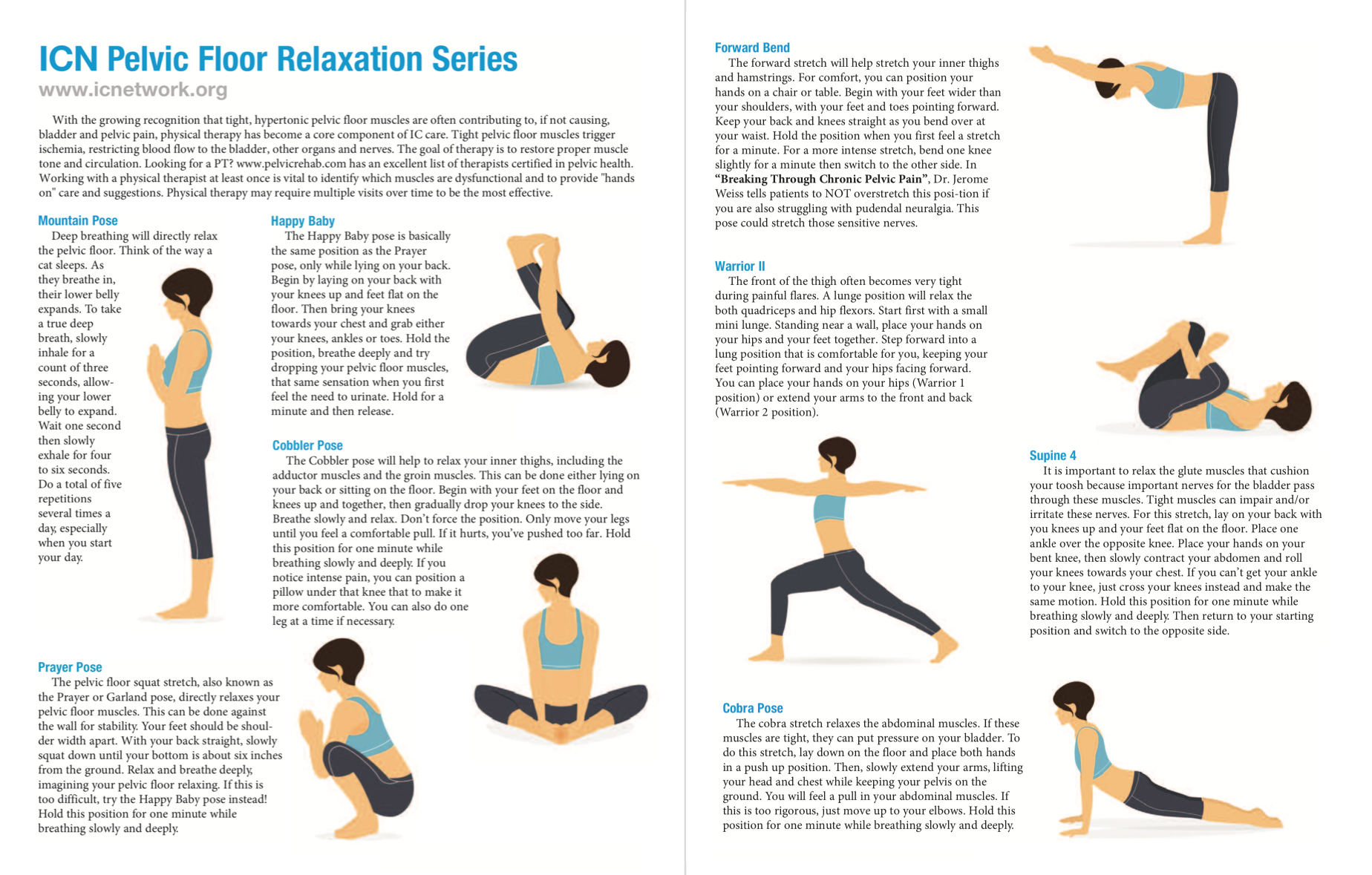
- STRETCHES – A healthy muscle is normally long, lose and pliant. When tense, muscles become short, stiff and painful. Listen to your body and reduce any muscle tension in your hips, butt, legs and back. Try some simple, easy stretches, deep breathing. Download our relaxation tips here!
- TAKE A WALK – Movement and gentle exercise release accumulated stress and improve circulation. If it’s not painful, take a walk around your house, your garden or your neighborhood. If you’re feeling comfortable with it, walk more quickly for an extra cardio benefit. You could also try a recumbent bicycle or even swimming. Avoid jogging or running.
- HEAT – In addition to using heating pads as described in the first section, try soaking in a warm bath tub but please do NOT use any harsh chemicals, bubble baths or soaps in the bath water which can irritate the sensitive skin in your crotch. Taking a warm bath every day is ideal for patients with chronic muscle tension.
- PRACTICE DEEP BREATHING
- TOPICALS – Some topical lotions and creams can reduce muscle tension, such as Tiger Balm, Neuroquell, ProSirona or some CBD products.
At 2-4 Hours: Getting serious about symptoms
- USE A GUIDED RELAXATION CD – We have several free relaxation recordings on our website that work well!
- MUSCLE RELAXANTS – Many physicians suggest a skeletal muscle relaxan, including: diazepam (Valium), cyclobenzaprine (Flexeril) and several others. Vaginal valium suppositories deliver medication to the pelvic floor region. These suppositories are usually made by a local compounding pharmacy on an as needed basis.
- HANDS ON THERAPY – If you are being treated for pelvic floor tension, then your physical therapist should have suggested exercises to reduce trigger points and muscle tension. This can involve stretching, applying pressure to various internal or external muscles with your fingers and by using vaginal dilators or wands.
At 24 Hours & Longer
- PHYSICAL THERAPY – Pelvic floor dysfunction often requires long term, consistent effort, usually with the help of a professional physical therapist. Myofascial physical therapy has a proven track record in fighting pelvic pain. If your pain does not responding to your home strategies, request a referral to a pelvic physical therapist for a treatment.
Stress & Anxiety Flares
Any patient can flare during periods of high stress and anxiety. Stress triggers the “fight or flight” response which prepares your body to fight or flee for your life. This then triggers pelvic floor tension, changes in blood flow, pain perception and more. When stress and anxiety is present for long periods of time, this can affect the entire body and has been linked to the development of chronic overlapping pain conditions (IC, IBS, vulvodynia, fibromyalgia, migraine, TMJ & others). Research studies now suggest that this occurs after trauma to the central nervous system, such as a major physical injury, abuse or bullying.
Triggers
- family illness, your illness, pain, loss of job, conflict at home or work, traveling
Rescue Plan
- Mind-Body Medicine Techniques (deep breathing, tapping, eye spy, etc.)
Pain Treatment May Be Required
Here’s an example that we often use in our phone support. You walk through your living room with a glass of water and see a flicker of flames at the bottom of your drapes. You walk out of the room and come back ten minutes later with that same glass of water, and see that your drapes are a raging inferno. At what point of time would that one glass of water stopped that fire?? Early! The same is true for managing IC flares and pain. The earlier you catch them, the easier it can be to stop them and the less it takes to stop them. Veteran patients often recognize their early warning signs (such as a specific type of pain) and catch the pain early.
Regardless of the trigger, some flares can provoke excruciating pain that requires treatment so that you are not suffering. Worse, grinning and bearing pain, allowing yourself to suffer and/or refusing to use medications may create even more neurosensitivity, including a condition called central sensitization. Pain should be treated promptly rather than be allowed to occur for extended periods of time.
Using pain medication can be controversial. Some urologists downplay the pain of IC and refuse to provide medication. Others are very compassionate and will help you find medication that can help you sleep and function better. In any case, a proper use of pain medication is not to escape life or “get high” but so that you can regain functionality in your daily, such as go to work, church, etc. There are a wide variety of pain medications that can help:
- Palmitoyethanolamide (PEA) is a simple fatty acid derived from eggs that has been found to reduce neuropathic pain. A 2019 study found that it significantly reduced pain in 87% of IC patients who tried it by month three with no side effects reported. It’s over the counter (PEAORA®), very affordable and a great option before considering pain medications that have more side effects.
- OPIOIDS – Opioids (i.e. Tylenol with Codeine, Morphine, etc.) are the mainstream of treatment for moderate to severe pain. Unfortunately, many physicians are now reluctant to prescribe them due to the opioid crisis. Available as oral medications, rectal suppositories, the 2022 American Urology Association IC/BPS Guidelines suggest that they can be used by patients with more severe pain, but should not be used as your only treatment for IC/BPS.
- ANTIDEPRESSANTS – Antidepressants have long been useful in the treatment of long-term chronic pain and appear to strengthen the body’s internal pain-fighting mechanism, improve the quality of sleep and may increase the effectiveness of other pain medications, including: amitriptyline, imiprimine, doxepin, desipramine, and nortriptyline. Talk with your doctor about potential side effects.
- ANTIHISTAMINES – Antihistamines (i.e. hydroxyzine) help reduce histamine-induced irritation in the bladder, particularly in patients with a history of allergies. When used with opioids, antihistamines apparently help to increase the pain-reducing action of the opioid.
- HYBRID PAIN MEDICATIONS – Tramadol (Ultram®) and tramadol with acetaminophen (Ultracet™) are prescription pain medications used for moderate pain. These weak opioids act on parts of the brain and spinal cord to reduce pain sensation.